HIV intervention information¶
Part of what makes EMOD such a powerful modeling framework is the flexibility and customization enabled by the campaign interventions. EMOD uses campaign files (see Campaign file for more information) to distribute the interventions necessary to facilitate disease eradication. This section is not intended to describe every available campaign for the HIV model; instead, it will highlight some of the most common interventions, and those that are essential for modeling HIV. For a complete list of all available interventions, see Campaign parameters.
Creating a health care system¶
Intervention campaigns in the EMOD HIV model typically involve health care, treatment, and access to care. Configuring campaigns involves the use of event coordinators, which determine who will receive the intervention; campaign events, which determine when and where interventions will be distributed; and the intervention itself, which determines what will be distributed. For HIV, these events and interventions can be configured to create a health care system, such that individuals with particular attributes are selected for particular types of care. For HIV, this system is termed the cascade of care, and involves testing, diagnosis, and treatment; individuals can leave and enter the cascade at multiple time points.
For more information on the cascade of care, see Cascade of care.
Diagnostics and testing¶
To route individuals into the care and treatment systems, it is necessary to use diagnostic testing. EMOD has multiple types of diagnostics, which can be found in Campaign parameters. The outcomes of different diagnostic tests can be used to initiate treatment, prevention services, entrance into health care systems, or lead to knowledge (such as HIV status) that will change the individual’s behavior. Testing can be triggered by a variety of factors, such as age, time of sexual debut, onset of symptoms, pregnancy, or simply through voluntary/routine testing. The triggers can be configured in the different types of diagnostics, and different results can be used to initiate care. Tests also have a probability of being wrong, such that some individuals that test negative may in fact be positive for the disease.
Decisions¶
Individuals can be enrolled in treatment due to the outcomes of diagnostic testing, but EMOD also allows for individuals to make decisions about treatment. These decisions can be based on factors such as time, age, the individual’s current state or sexual debut status, or even a random choice.
For individuals making a random choice, EMOD will base the decision on a random coin flip, or if more than 2 choices are configured in the campaign file, a dice roll. All choices and their outcome probabilities are configurable; should the sum of the probabilities not equal 1, then EMOD will normalize the sum to 1, while keeping their relative proportions the same.
Some classes of interventions contain a Choices parameter, where the user can configure an array of options and the probabilities for each outcome. In those cases, the probabilities are not dependent on the number of choices, but must still sum to 1.
Configurable history of past treatment guidelines¶
The results of diagnostic tests are used to route individuals to treatment, with target levels for CD4 counts, WHO stage, or other factors used to determine the course of action for the individual. Over the past several decades, such treatment guidelines have changed, and EMOD allows for these changes in guidelines to be incorporated into the diagnostics. For example, cut-off values for CD4 counts by age and pregnancy status to determine eligibility for treatment have expanded in South Africa over the past 20 years. Configuring InterpolatedValueMap (which consists of arrays of Times and Values) for their appropriate parameters will let the model utilize these different diagnostic levels in the appropriate years.
The below JSON example shows the HIVARTStagingCD4AgnosticDiagnostic intervention class, where several parameters demonstrate configuring past history guidelines. For example, Adult_By_WHO_Stage has different WHO stage category recommendations for ART eligibility depending on year, and Child_Treat_Under_Age_In_Years_Threshold shows how the age at which children were eligible for ART changed over time.
{
"class": "CampaignEvent",
"Event_Name": "OnART1-triggered piecewise event",
"Start_Day": 1,
"Nodeset_Config": {
"class": "NodeSetAll"
},
"Event_Coordinator_Config": {
"class": "StandardInterventionDistributionEventCoordinator",
"Event_Name": "DrawBlood constant test, broadcasts HIVPositiveHIVTest",
"Demographic_Coverage": 1,
"Intervention_Config": {
"class": "NodeLevelHealthTriggeredIV",
"Trigger_Condition_List": ["HIVNeedsHIVTest"],
"Demographic_Coverage": 1,
"Duration": 14600,
"Actual_IndividualIntervention_Config": {
"class": "HIVARTStagingCD4AgnosticDiagnostic",
"Positive_Diagnosis_Event": "HIVPositiveHIVTest",
"Base_Specificity": 0,
"Base_Sensitivity": 0,
"Cost_To_Consumer": 10,
"Days_To_Diagnosis": 5,
"Disqualifying_Properties": ["InterventionStatus:InterventionStatus_1", "InterventionStatus:InterventionStatus_2", "InterventionStatus:InterventionStatus_3"],
"New_Property_Value": "InterventionStatus:InterventionStatus_4",
"Individual_Property_Active_TB_Key": "HasActiveTB",
"Individual_Property_Active_TB_Value": "YES",
"Adult_Treatment_Age": 1865,
"Adult_By_WHO_Stage": {
"Times": [
1990, 1995, 2000, 2005
],
"Values": [
4.1, 2, 3, 4
]
},
"Adult_By_TB": {
"Times": [
1990, 1995, 2000, 2005
],
"Values": [
0, 1, 1, 1
]
},
"Adult_By_Pregnant": {
"Times": [
1990, 1995, 2000, 2005
],
"Values": [
1, 1, 1, 0
]
},
"Child_Treat_Under_Age_In_Years_Threshold": {
"Times": [
1990, 1995, 2000, 2005
],
"Values": [
1, 2, 5, 3.2
]
},
"Child_By_WHO_Stage": {
"Times": [
1990, 1995, 2000, 2005
],
"Values": [
1.1, 1.5, 2, 2.5
]
},
"Child_By_TB": {
"Times": [
1990, 1995, 2000, 2005
],
"Values": [
1, 1, 1, 0
]
}
}
}
}
}
Restricting multiple entries into health care¶
Health care in EMOD is bi-directional: it can be applied to individuals, or it can sought by individuals in response to various triggering events including birth, sexual debut, pregnancy, or AIDS symptoms. A potential problem created by this structure is that an individual could end up in care multiple times. For example, an individual might have an antenatal care (ANC) visit and, in the same time-step, seek health care for AIDS symptoms, both leading to HIV testing and staging.
The HIVMuxer intervention is a method that can be used to prevent this problem. HIVMuxer counts the number of times an individual is simultaneously waiting in the same delay state or group of delay states and restricts the number of entries that individual is eligible to receive.
Antiretroviral therapy (ART)¶
Survival time for untreated HIV is described in Intrahost dynamics and HIV biology, with individuals progressing through the three diseases stages (acute, latent, AIDS). Antiretroviral therapy (ART) significantly alters this progression and impacts survival in a positive way (for more information on ART, see HIV disease overview). In EMOD, survival time on ART is assumed to follow a Weibull proportional hazards model published by May et. al. with the IeDEA Southern Africa collaboration [Ref32]. The hazard ratios are applied proportionally to weight and CD4 count (at initiation of ART for both), and are applied categorically to WHO stage (at initiation of ART), gender, and age. Body weight is assumed to be linked to WHO stage progression, with linearly declining body weight between each transition.
The hazard ratios are shown in the following tables:
Category |
Hazard ratio base |
Hazard ratio multiplier |
|---|---|---|
Body weight at initiation |
21:1 |
0.93 per kg |
CD4 count at initiation |
1:32 |
0.9925/cell/uL up to 350 cells/uL |
Continuously applied hazard ratios
The reduction in hazard of death per increase in CD4 count is capped at a CD4 count of 350 cells/uL, such that individuals initiating at CD4 counts greater than 350 cells/uL receive the same CD4-related hazard adjustment as those with a CD4 count of 350 cells/uL. In other words, the model currently makes a conservative assumption that the health benefit of initiating at CD4 counts greater than 350 cells/uL is identical to that of initiating at exactly 350 cells/uL.
Category |
Value |
Hazard ratio |
|---|---|---|
WHO stage |
3 or 4 |
2.71 |
Gender |
Female |
0.68 |
Age |
>40 years |
1.43 |
Categorically applied hazard ratios
There are multiple campaign classes that are used to implement ART programs in the model. To enroll individuals on ART, the ARTBasic intervention is applied. To remove individuals from ART, the ARTDropout intervention is applied. Note that both of these interventions will only impact individuals that are HIV+; in order to use ART as a prophylactic, the SimpleVaccine class must be used (see Pre-Exposure Prophylaxis). Finally, eligibility for ART can be determined through two classes, HIVARTStagingCD4AgnosticDiagnostic and HIVARTStagingByCD4Diagnostic. When using CD4-dependent ART interventions, it is important to use the HIVDrawBlood intervention first, as this acts analogously to performing phlebotomy and logs an HIV-infected individual’s current CD4 count.
Note that the multiplicative effect of ART for reducing HIV transmission is set in the configuration file, while the campaign interventions used determines who receives the effects of ART and at what time periods. See Transmission for more information on HIV transmission and the factors that influence it.
ART’s impact on CD4 count¶
CD4 count declines with advancing HIV disease progression, but CD4 counts can be reconstituted with ART. The Swiss HIV Cohort Study demonstrated that absolute changes in CD4 counts from the baseline measurement are consistent over the first few years of ART, independent of the baseline value. For example, a patient starting with a CD4 count of 100 cells/uL, will, on average, reconstitute to 200 cells/uL in the same time that a patient starting at 200 cells/uL will reconstitute to 300 cells/uL. This reconstitution rate follows a quadratic increase that saturates over three years, and can be calculated with the equation,
CD4 count increase = 15.584 x (months since initiation) - 0.2113 x (months since initiation)^2
Interruption of ART will initiate a decline in CD4 count, and resumption of ART will then initiate another reconstitution of CD4. EMOD calculates survival time on ART discontinuation by first determining what the survival time would have been for a newly infected individual at the age when discontinuation occured, and then adjusts the time to account for potentially low CD4 at discontinuation using the following equation:
% survival time applied at ART discontinuation = (CD4 at discontinuation)/(CD4 at infection)
The slope of CD4 decline is comparable to a newly infected individual, but the infection is “fast-forwarded” proportionally to the loss of CD4 count relative to a newly infected individual.
When ART is re-initiated, survival is drawn from the distribution corresponding to the updated CD4 count and age at re-initiation. Mortality rates on ART are modeled as Weibull distributions with a shape parameter <1, which produces a “super-exponential” mortality curve (i.e. one with a probability density function that declines more rapidly than an exponential distribution). This produces an elevated mortality rate soon after ART initiation, and a lower mortality rate as time on ART increases. Discontinuation and re-initiation of ART produces higher mortality rates than continuous ART by repeatedly exposing the individual to this high early mortality rate.
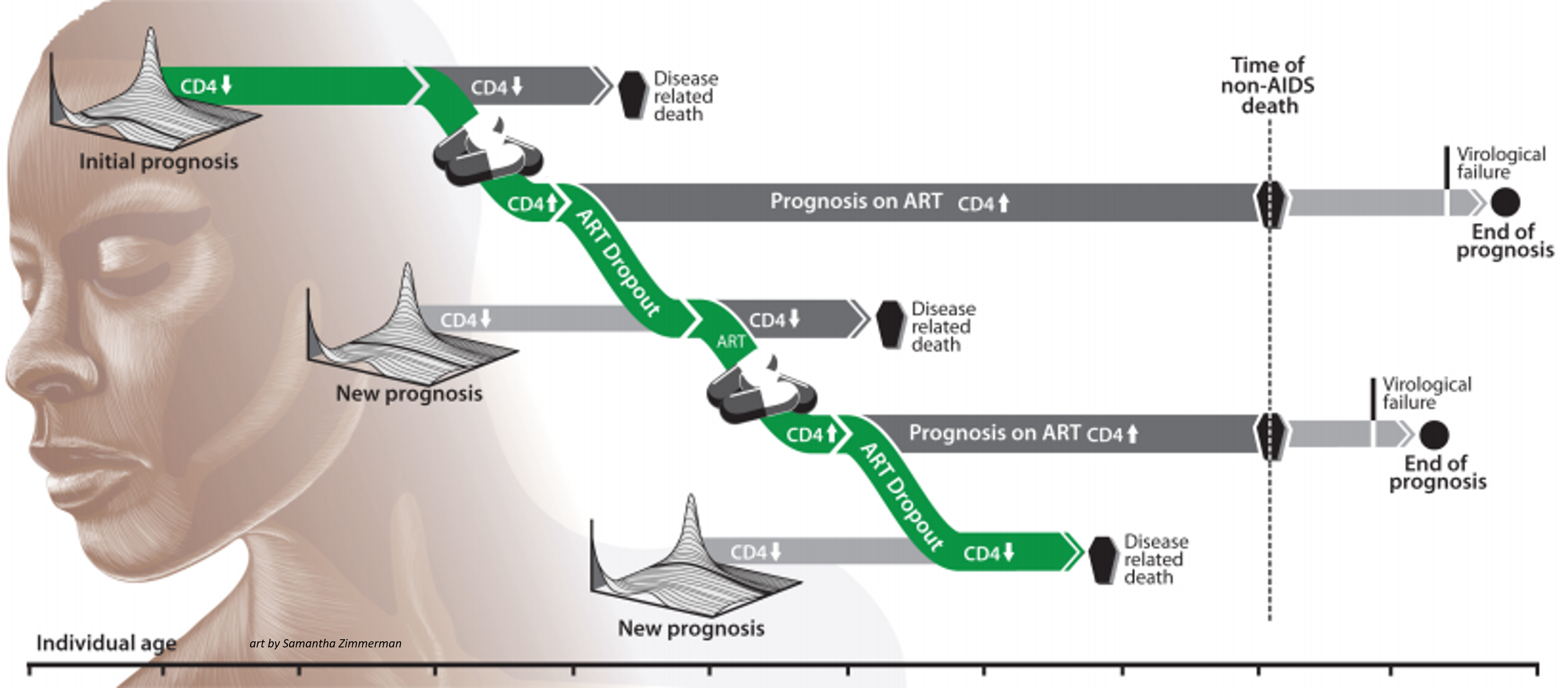
An example of CD4 counts and prognosis for a patient on and off ART. Art by Samantha Zimmerman.¶
Pre-Exposure Prophylaxis¶
Antiretroviral therapy as treatment for HIV was explained above, in Antiretroviral therapy (ART). ART can also be used as Pre-Exposure Prophylaxis (PrEP), to prevent the transmission of HIV. In EMOD, the ART interventions are only used for treatment for HIV+ individuals, so to use ART as a prophylactic, it is treated as a “vaccine” and the vaccine intervention classes are used.
Prevention of mother-to-child transmission (PMTCT)¶
HIV may be transmitted vertically, from mother-to-child as explained in Transmission. To prevent this mode of transmission, there is a campaign intervention (see PMTCT in Campaign parameters) that will modify the probability of transmission from an HIV-infected mother that is not on suppressive ART. The Efficacy parameter is used to modify the configuration parameter that determines the probability of maternal transmission. The MTCT rate is independently calculated for each pregnancy because the PMTCT intervention automatically expires 40 weeks after it is distributed. At this time, the efficacy is reset to 0.
Condom use¶
The probability of condom usage is independently configured for each relationship type, as explained in Relationships and contact networks. Condom usage impacts HIV transmission probabilities through a modifier (see Transmission). In addition to the configuration parameters, condoms can also be distributed through a campaign intervention, STIBarrier. This campaign overrides the probabilities of usage set in the config.json files with new parameters. The relationship is still a time-varying sigmoidal probability.