Multidrug-resistant TB¶
Multidrug-resistant TB (MDR-TB) is disease involving a strain of M. tuberculosis that is resistant to at least two of the four drugs in the standard first-line regimen, isoniazid and rifampicin. Researchers believe such strains occur naturally during infection at low frequencies. However, the use of four drugs in the standard first-line regimen, each with a different mode of action, typically ensures that such strains do not replicate to high frequencies in an infected individual.
Drug resistance arises when inappropriate treatment undermines the efficacy of first-line treatment. When this occurs, M. tuberculosis strains resistant to one or more drugs may replicate at high frequencies and become the predominant strain in an infected individual. From an epidemiological point of view, this presents two difficulties: not only are individuals who have acquired a drug- resistant M. tuberculosis strain more difficult to treat, but they may also transmit the drug- resistant strain to others. Resistance to INH and RIF commonly co-occurs in the same individual, accounting for the inclusion of these drugs in the definition of MDR-TB.
When drug resistance occurs in individuals who are initially infected with a drug-sensitive strain and then acquire MDR-TB through ineffective treatment, it is called secondary drug resistance. When MDR- TB is transmitted directly to an individual (the initial infection is with a drug-resistant strain), it is called primary drug resistance.
In EMOD, you can set parameters for the rate at which each specific drug treatment leads to resistance. This is set alongside related drug parameters that control the rate at which cure, inactivation, mortality, and relapse occur. If you are using AntiTBDrug, you will set these values in the campaign file as part of the intervention itself. If you are using TBHIVConfigurableTBdrug, you will set these values in the configuration file under TBHIV_Drug_Params (see Drugs and treatments parameters for more information) and list just the drug name in the intervention. All rates are specified as a probability per time step. Both interventions also include parameters for setting the reduction in transmissibility while on treatment.
The different base strains and substrains in a simulation, whether they differentiate between drug- sensitive and drug-resistant TB or others, are specified using Number_Basestrains and Number_Substrains in the configuration file and Antigen and Genome in the outbreak event in the campaign file.
In general, drug-resistant strains of any pathogen (including those for TB) are assumed to have a lower fitness and infectiousness than wild-type, drug-sensitive strains, especially in the absence of drug pressure. You can xplore the effect of reducing MDR fitness in the model by setting TB_MDR_Fitness_Multiplier to less than one in the configuration file (see Infectivity and transmission parameters).
The following sections provide a few examples of MDR-TB scenarios. To run these simulations yourself, see the TB/MDR-TB scenario in the downloadable EMOD scenarios zip file. Review the README files there for more information.
Ineffective treatment¶
Ineffective treatment is common in resource-limited settings that lack the capacity to diagnose MDR- TB or the means to provide expensive second-line treatments. Often, following inappropriate treatment for drug-sensitive TB and acquisition of MDR-TB, infected individuals seek additional treatment. However, in the absence of MDR-specific second-line treatments, these individuals received a second round of the same ineffective treatment. In general, treatment initiated in the absence of a full diagnosis is called “empiric treatment” and has previously been recommended by the WHO for MDR-TB.
The effect of treatment on the infectiousness of MDR-TB is largely unknown. You can explore different assumptions regarding infectiousness while on treatment using Reduced_Transmit in the intervention configuration.
Acquired MDR-TB¶
In the first scenario, Ineffective_Treatment, the campaign file specifies that all individuals are infected with drug-sensitive TB and provided with ineffective treatment that leads to resistance in approximately 10 days (0.1 probability per day). See how the entire population eventually acquires MDR-TB.
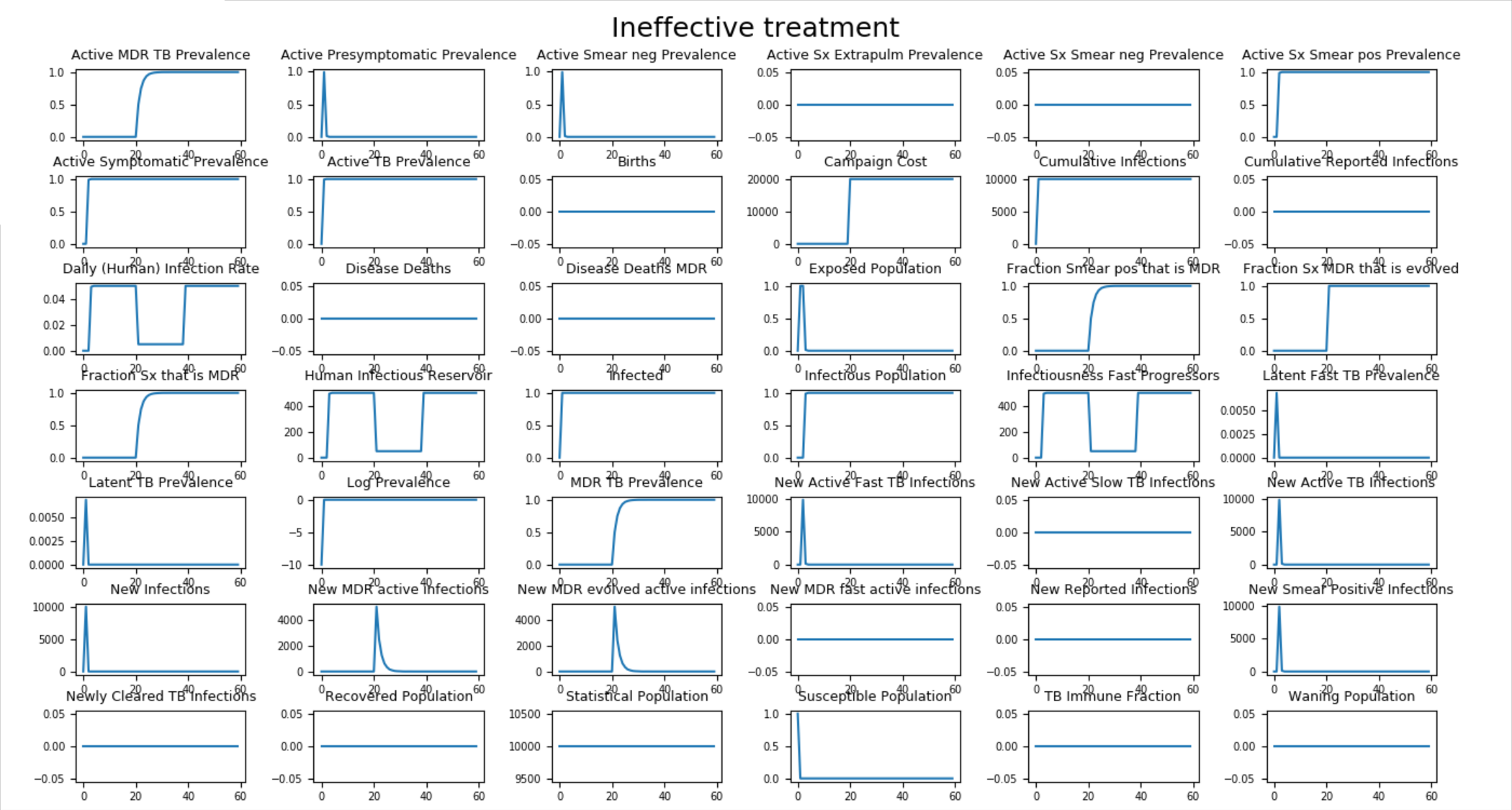
Figure 1: Population acquires MDR-TB (secondary drug resistance)¶
Transmitted MDR-TB¶
If the campaign file is modified to reduce the size of the initial outbreak and add a second round of empiric treatment for individuals who fail treatment (those who experience no change in disease state), most cases of MDR-TB are transmitted (primary drug resistance). In the figure below, only 1% of the population is infected by the initial outbreak and the additional round of empiric treatment has minimal impact on the course on the spread of MDR-TB.
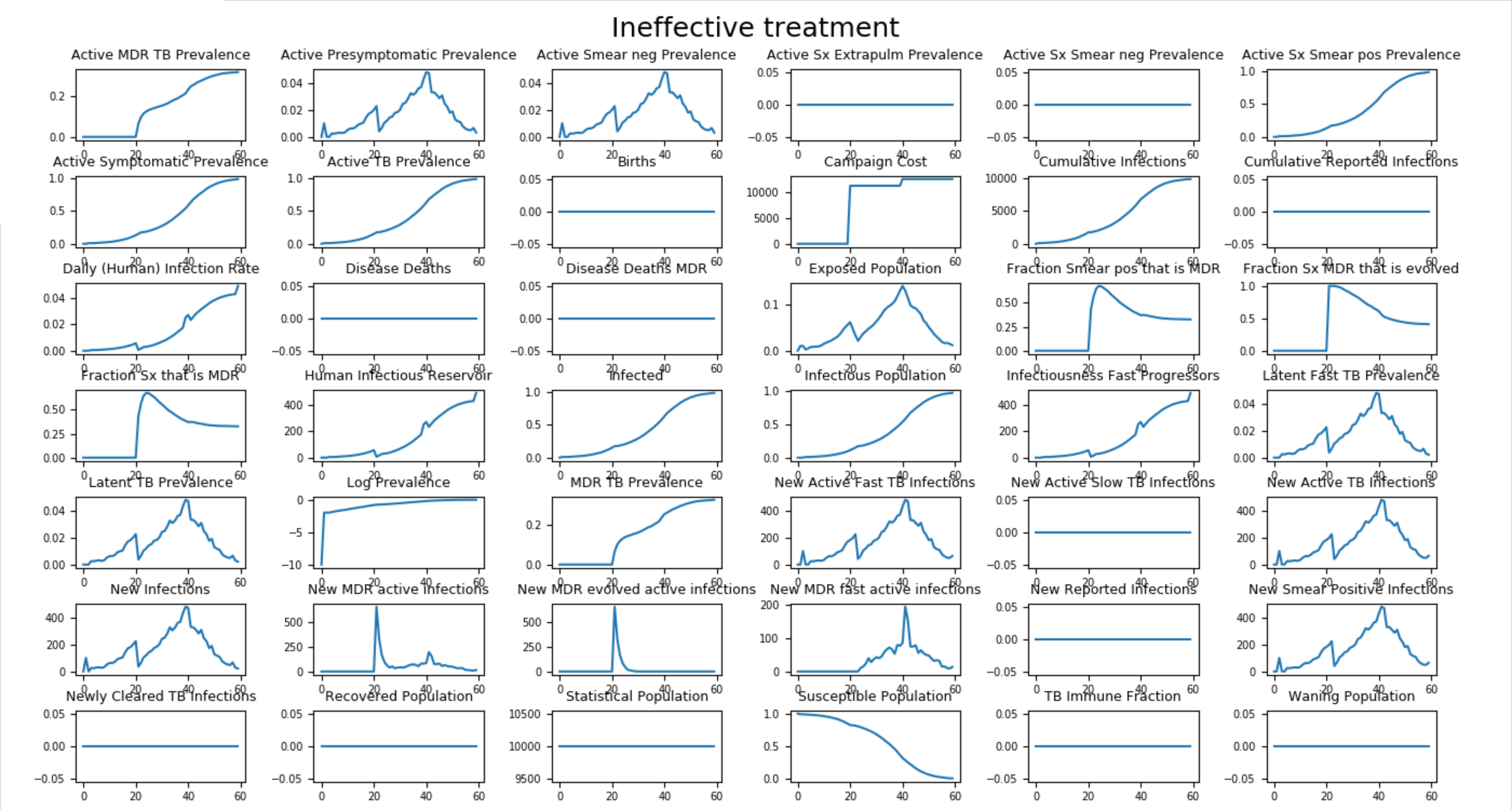
Figure 2: Population transmits MDR-TB (primary drug resistance)¶
Effective treatment¶
In the second scenario, Effective_Treatment, individuals who fail drug treatment are tested for MDR- TB prior to receiving additional treatment. If the test is positive, they receive the appropriate second-line drug regimen for drug-resistant strains of TB.
The figure below shows how the addition of testing and appropriate second-line treatment does a much better job of controlling the spread of MDR-TB.
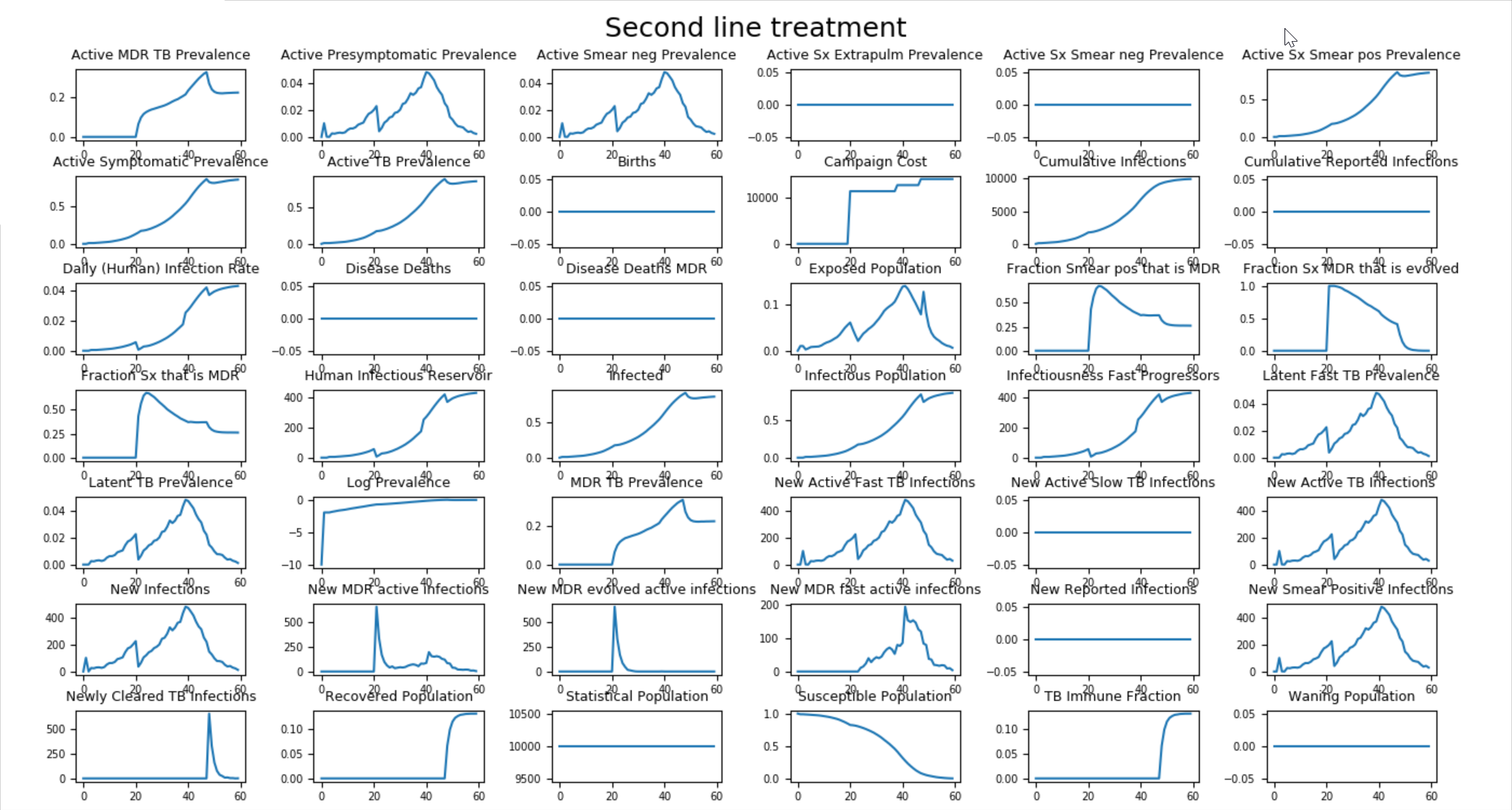
Figure 3: Testing and treating appropriately for MDR-TB¶